Got chronic knee pain? Has a knee replacement come up in conversation? Bet this sounds familiar…
You’ve been having severe pain and stiffness in your knee after a car or sports-related injury, tumor, fracture, or just with normal joint wear and tear. Your pain prevents you from sleeping well. Maybe your knee buckles on you when you are trying to walk or climb the stairs. It’s time to get help.
You decide to schedule an appointment with your primary care doctor, and they refer you to an orthopedist. Upon examination and/or an x-ray at the doctor’s office, the orthopedist informs you that you have end-stage knee arthritis, or joint inflammation.
The orthopedist prescribes anti-inflammatories and/or gives you a steroid or lubricating injection for relief. Some stories end here.
But for others, after several months, the severe pain and stiffness return.
Maybe you’ve tried physical therapy and it’s worked for you. Some stories end here, too.
But maybe you’ve been trying to maintain the health of your knee for a while, and although therapy decreases the pain and allows you to move better, symptoms persist. You can’t catch a break.
So, what’s next!?
You follow-up again with your orthopedist, and at this point they recommend a total knee replacement (TKR) or partial knee replacement (PKR).
But what exactly is a knee replacement, and what does recovery look like? How can it help you get back to doing the things you love?
Knee Replacements: Total vs Partial
A TKR or PKR is a surgical procedure performed by an orthopedic surgeon to replace damaged bony surfaces and cartilage, or the cushion between your joints. Your doctor may also refer to these procedures as a total knee arthroplasty (TKA) and uni-compartmental knee arthroplasty (UKA).
During a partial knee replacement or UKA, only one side or compartment of the knee joint is replaced. During a total knee replacement, both sides, referred to as the medial (inside) and lateral (outside) compartments are replaced.
Your doctor determines which version is appropriate for you based on your imaging and symptoms.
Who is Appropriate for a Knee Replacement?
Individuals with moderate to severe pain and stiffness, limited mobility, and chronic inflammation and swelling may be candidates for a knee replacement. Those who do not respond to conservative management such as steroid or lubricating injections, anti-inflammatories, other surgeries, or physical therapy may also be candidates for a knee replacement. Knee replacements are commonly performed in individuals 50 to 80 years of age. They have also been done successfully in juveniles and young adults, and can last about 15 to 20 years.
With proper care after a knee replacement, including physical therapy, you can get back to the things you love doing, with a recovery time of usually 2-3 months.
At this point, you and your doctor have decided a knee replacement is right for you. Congratulations, you are one step closer to scoring 90 strokes on 18 holes!
Here’s what you need to know before your surgery.
Knee Joint Anatomy
The knee joint is made up of three bones: the femur (lower end of the thigh bone), patella (knee cap), and tibia (shinbone). The medial and lateral menisci are cartilage surfaces that sit between the bones. They act as shock absorbers and allow for smooth movement/gliding of the bony surfaces when bending and straightening your knee.
- Knee Joint – Front View
Image courtesy of Complete Anatomy
Without sufficient cartilage, space between the bony surfaces, or with excessive swelling (inflammation) caused by conditions such as osteo- or degenerative arthritis, rheumatoid arthritis, post-traumatic arthritis, or juvenile arthritis, pain, stiffness, and limited mobility can occur.
The knee joint also has several other types of tissues that help to provide stability to the knee, and therefore prevent wear and tear on the joint. Ligaments, which connect bone to bone, such as the medial and lateral collateral ligaments (MCL and LCL), anterior cruciate ligament (ACL), and posterior cruciate ligament (PCL) prevent excessive movement at the knee joint and therefore injury.
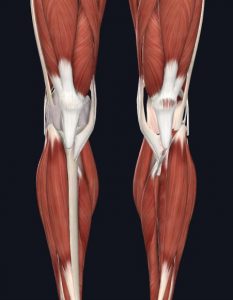
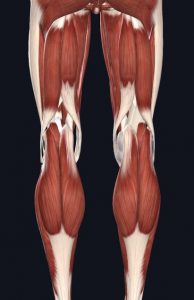
Muscles such as the quadriceps (front thigh muscles) and hamstrings (back thigh muscles) and their tendons, which attach the muscles to the bony surfaces of the knee, also help to accelerate, decelerate, and control movement to prevent injury. Damage to any of the stabilizing structures of the joint, or weakness in the quadriceps or hamstring muscles can promote improper joint loading, cause deformity, and result in excessive wear and tear and/or injury.
- Muscles of Knee – Front
- Muscles of Knee – Back
Images courtesy of Complete Anatomy
Now that you’ve read about the anatomy of the knee joint, here’s what to expect before, during, and after your surgery.
What to Expect Before Your Surgery
Besides learning as much as you possibly can about your surgery beforehand, previous patients who have gone through the process cannot stress enough the importance of attending prehab!
Prehab is typically a single physical therapy visit (or more depending upon your individual needs and limitations). A licensed physical therapist will assess your knee, including range of motion and strength, to determine your baseline. He/she will teach you how to get around safely after surgery, and what exercises you should perform before returning for your first physical therapy session after the procedure (post-op rehabilitation).
If you want to learn more about prehabilitation services, call our office for more information!
It’s Surgery Day!
Depending upon your surgeon, the procedure will either be outpatient (you go home the same day) or inpatient (you remain in the hospital a few days). Check out Island Orthopaedics or Minimally Invasive Surgery Hawaii for more information.
Make sure you know what to expect so you can plan ahead. What type of assistive device do you need as you leave the hospital? Will you need help when you get home? Find out as much as you can and discuss this with your therapist during prehab.
During a knee replacement surgery, the entire knee is not replaced as the name might suggest. Only the bony surfaces are “cleaned-up” and replaced. Usually a large incision is made along the front of the knee where the surgeon will cut through the quadriceps muscle, tendon, patellar ligaments.
Surgeons may have different approaches. If you’re curious about specifics, it’s best to ask your surgeon. However, surgeons perform the following general steps:
- The damaged portions of cartilage are removed along with some of the underlying bone if necessary to prepare the bone for insertion of the replacement or implant.
- The implant is positioned appropriately to your anatomy. These metal parts may be cemented or “press-fit” into the bone.
- Depending upon the degree of damage, the underside of the patella (knee cap) may be resurfaced.
- Finally, a medical-grade plastic spacer is inserted between the metal components to create a smooth gliding surface.
Here is an animated video of the full procedure from YouTube if you want to know more.
General Recovery Time After a Total/Partial Knee Replacement
How long after your knee replacement do things start to feel “normal”? As all physical therapists say: it depends! Every person’s recovery journey is different. Here’s a general explanation of what to expect.
Depending upon your surgeon, you will go home with a bandage and stitches, staples, glue, or tape strips over the surgical incision. At your first follow-up appointment, your doctor or an assistant will give you further instructions on how to care for your wound. If you have stitches or staples, your doctor or their assistant will remove them usually within 10 to 21 days after your surgery.
You will typically develop a scar at the incision site after surgery, which is completely normal. Your physical therapist will show you how to perform scar tissue mobilization to decrease its appearance and ensure the tissue is moving properly after the incision site has fully healed at the 6 to 8 week mark.
It is always important to monitor your incision site for any signs of infection. Also monitor your leg for signs of a blood clot, also known as a deep venous thrombosis (DVT). Your physical therapist will educate you on things to look out for at your prehab appointment.
You may require use of an assistive device to get around – a cane, crutches, or a walker – for 1 to 3 weeks after your surgery due to pain and stiffness. Most individuals are able to walk on their own about 4 to 8 weeks after surgery. During your prehab appointment(s), your physical therapist will instruct you on correct use of your assistive device. Following up with a physical therapist after surgery, usually within the first week, is crucial to ensure you get back to walking normally after surgery. Do not wait.
It is very normal to experience pain, stiffness, and swelling after the surgery. You may have difficulty finding a comfortable sleeping position or sleep throughout the night. It is normal for swelling to linger for 3 to 6 months. In early rehab, you will learn how to manage the swelling and how to find a comfortable sleeping position.
Exercises to Master for Better Recovery
During your course of care, your physical therapist will teach you individualized exercises that target your specific limitations. Nearly everyone has the same goal at the beginning of therapy: get the knee moving!
It can be difficult to get the knee moving right after surgery, but it’s important. Getting to a physical therapist as soon as possible can help knee movement feel more comfortable over time. Sticking to your exercises will help you feel better faster, even if they’re difficult at first.
Two common exercises prescribed at the onset of your care are quad sets and heel slides. These work on straightening and bending – they’re crucial to your full recovery.
1. Quad sets work on strengthening the quadriceps (front/anterior thigh) muscle. It is responsible for straightening the knee, and plays a large role in your single leg balance, squatting, and stair-climbing. They can be performed lying on your back, sitting with your legs outstretched in front of you, or standing and with/without a towel roll under your knee or ankle. Hold times and repetitions will vary depending upon your needs.
2. Heel slides work on bending the knee. It is important to restore normal mobility for squatting, stairs, etc. and help to decrease swelling in the knee. Perform these lying on your back or sitting and with/without a strap or towel. Hold times and repetitions will vary depending upon your needs.
Reach out!
JACO Rehab wishes you the best of luck with your upcoming surgery. We encourage you to reach out to us with any questions!
Call (808) 381-8947 or e-mail info@jacorehab.com for more information.
Written by Jenn Lewis, DPT