Back pain is an very common condition. Almost 80% of people experience back pain at some point in their lifetime. (2) It can be scary, especially when you’re in a great deal of pain.
One of the most commonly diagnosed reasons for back pain is the discovery of a herniated disc. If this is you, don’t worry. There’s a lot of evidence out there that points to positive outcomes with conservative care.
Physical therapy for herniated discs is one of the front-line approaches to symptom management. Reach out to JACO Rehab on Oahu and get an evaluation!
What is a Lumbar Disc?
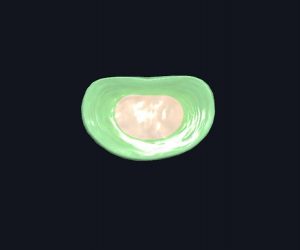
Your spine has spacers between each vertebrae. Those are your spinal discs. You have spinal discs in your neck, thoracic region, and lumbar region.
- A Lumbar Disc (highlighted)
Images courtesy of Complete Anatomy
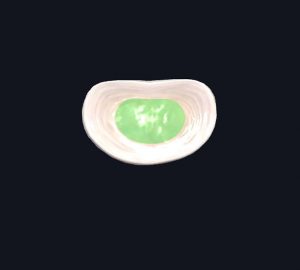
All spinal discs are made up of a fibrous outer ring and a more gelatinous center. Their main purpose is to act as a shock absorber for the spine so that it can handle loads, particularly compression and bending.
- Anulus Fibrosis (fibrous outer layer)
- Nucleus Pulposus (gelatinous inner layer)
Images courtesy of Complete Anatomy
Your lumbar discs experience the least amount of stress when laying down, and the most amount of stress when sitting with poor posture or lifting something heavy with a bent, unstable back position.
Discs are sensitive structures to inflammation. (1) When they’re excessively stressed, they can cause pain. Prolonged sitting or lifting excessive weight with poor form can cause a herniation (or make an existing one feel worse). Laying down flat can make symptoms feel better.
Pinched Nerve vs. Herniated Disc
Before understanding a treatment approach or healing timeline, it’s important to understand how a herniated disc relates to your symptoms.
It’s common to hear a herniated disc interchanged with a “pinched nerve.”
A herniated disc can “pinch” a nerve, but a pinched nerve is not always due to a herniated disc.
A pinched nerve generally refers to when the nerve has something pressing on it, causing irritation. A number of things can irritate a nerve this way, including:
- a herniated disc
- an osteophyte/bony growth
- a cyst
- a narrowing canal (usually referred to as stenosis)
Even muscles or soft tissue restrictions can irritate a nerve somewhere along the its path.
However, a disc injury doesn’t always have to involve the nerve. Sometimes the disc’s structure can be disturbed, causing an “annular tear” or a tear in its fibrous ring. Since discs can signal inflammation, that can be enough to cause discomfort.
If the gelatinous structure in the center of the disc protrudes out of a tear, a nerve is more likely to be involved. This is because the disc is now encroaching on the nerve’s space, “pinching” it to the point of irritation. The “severity scale” of a herniated disc’s structural disturbance is discussed in the next section.
But, in many cases, disc herniations cause no pain at all. Many people are walking around with some level of disc disruption and don’t even know it.
Stages of a Disc Herniation
There are a 4 stages of a herniated disc.
- Degenerative: some disruption of the fibrous ring, no herniation
- Prolapse
- Extrusion
- Sequestration: some gelatinous substance has left the disc completely, definitely herniated
This is not a scale for pain. You could have no pain but have a sequestration. You could have a lot of pain but have only a small prolapse.
However, the closer you are to sequestration, the more likely you are to have nerve involvement.
What Are the Symptoms of a Herniated Disc?
A disc disruption can cause central low back pain with burning, stinging, generalized discomfort. If a disc has herniated and is encroaching on a nerve, it can cause pain, weakness, or altered sensation into the leg.
Symptom location depends on the level affected. When a physical therapist evaluates the location, we are looking for “myotomal” and “dermatomal” patterns for clues.
- Myotomal Patterns: Muscular weakness due to abnormal nerve conduction along a nerve’s specific path.
- Dermatomal Patterns: Altered sensation due to abnormal nerve conduction to along a nerve’s specific path. This can include burning, coldness, tingling, numbness, or pain.
Tracing myotomal and dermatomal patterns back to the origin can reveal which level is affected, even without an MRI.
Sometimes symptoms come and go. This is very typical of nerve involvement, as nerves can be very fickle.
You’ll hear physical therapists discuss centralization and peripheralization. If your discomfort is spreading to the periphery, or peripheralization, it means that symptoms are worsening. Symptoms in more places is not the goal! We want to find ways to centralize your symptoms, or chase them back to its origin.
Even if your pain is increased but it’s in less places, that’s considered a win.
It’s important to track what centralizes and what peripheralizes your symptoms. That information can help your physical therapist teach you how to avoid aggravating movements or positions while the nerve calms down.
Can a Herniated Disc Heal Itself?
There have been several relatively new research and case studies that have reported complete resorption of a herniated disc.
Yes, discs can heal themselves over time!
Surgery is not often necessary right away unless there are major neurological deficits, like loss of bladder function. Conservative care is the first option in most cases because there is a good chance of recovery. Some cases will require surgery if conservative care isn’t enough, but you’ll still need physical therapy after your procedure to regain strength and mobility.
Studies have shown that even the worst of the herniations – sequestrations – can heal over time. In one study, only four of the thirty-seven patients needed surgery. Fully sustained recovery required almost two years. (3) However, just because it took time for full recovery, doesn’t mean that patients weren’t returning to their normal activities before the two year mark.
A different study followed a 25 year-old man’s healing time after a herniated disc. After five months of conservative care, his symptoms decreased. (4) After two years, he returned for a follow-up. He reported no recurrence in pain since treatment, and the MRI revealed improvements in structural integrity. Eight months later, the MRI revealed a “normal” disc.
Remember that an MRI’s abnormal findings does not have to be symptomatic. You can be healing functionally, displaying no symptoms, but still showing an abnormal MRI.
It takes time, but a herniated disc can have the capacity to heal itself under supervision and care. Sometimes, if a disc is causing severe neurological problems such as bowel or bladder issues, surgical approaches may be best. It’s important to discuss your specific options with a doctor and your physical therapist.
Physical Therapy for Herniated Discs
Conservative treatment for herniated discs almost always involves physical therapy.
Your physical therapist will work with you in understanding your symptoms and how to treat your condition. As stated earlier, you’ll learn the best ways to centralize your symptoms in an effort to decrease nerve irritation (if applicable). Then, you’ll learn how to maintain progress while getting back to your normal life.
While you’re waiting to see a physical therapist, there is one movement that may help alleviate symptoms: lumbar extension!
The best way to start is to offload your spine by laying down. Then, assume the “cobra stretch” position (see below). Pay attention to your symptoms: is there relief?
Here’s a great example of one of our therapists relieving her back using the “cobra stretch” after rowing in her outrigger!
Tip: This could feel intense. Try starting on your stomach and propping yourself on your elbows to start.
If you’ve tried this and it helped, be sure to tell your physical therapist as it can help in developing a treatment plan based on directional preferences, which they may discuss with you.
What Should You Not Do for a Herniated Disc?
The easy answer: If it causes more symptoms, don’t do it.
But life goes on, and you have to manage. Your physical therapist can help you problem-solve daily activities to make them less difficult and encourage further healing.
Remember: Discs are loaded with compression and bending. It’s best to avoid compression and bending positions at first, then slowly reintroduce bending movements when you’re ready.
Don’t worry, your body will be able to tolerate bending again, although many of the movements that likely caused the pain in the first place are generally regarded as “bad form”.
Here are examples of compression and bending positions to avoid:
We are all guilty of these!
Instead of sitting slouched, try using a chair with lumbar support to keep your spine in a more neutral position. Standing breaks at work are useful if you sit at a desk.
When reaching for low items or lifting, use your legs and not your back. You’ll want to squat instead of bending forward at your lumbar spine.
Reach Out!
If you’re still unsure what is best for you, consult with your physical therapist! Reach out to JACO Rehab today and get physical therapy for your herniated disc.
Written by Nicole Hernandez, DPT
References
1. Amin RM, Andrade NS, Neuman BJ. Lumbar Disc Herniation. Curr Rev Musculoskelet Med. 2017 Dec;10(4):507-516. doi: 10.1007/s12178-017-9441-4. PMID: 28980275; PMCID: PMC5685963.
2. Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354(9178):581–585. doi: 10.1016/S0140-6736(99)01312-4.
3. Benson RT, Tavares SP, Robertson SC, Sharp R, Marshall RW. Conservatively treated massive prolapsed discs: a 7-year follow-up. Ann R Coll Surg Engl. 2010 Mar;92(2):147-53. doi: 10.1308/003588410X12518836438840. Epub 2009 Nov 2. PMID: 19887021; PMCID: PMC3025225.
4. Wang R, Luo H. Regression of lumbar disc herniation with non-surgical treatment: a case report. Journal of International Medical Research. June 2021. doi:10.1177/03000605211020636