Slowly developing discomfort by the heel or arch of your foot? Uh, oh… could the beginnings of a stubborn injury called plantar fasciitis.
If you’re catching the symptoms early, you still have an opportunity to reverse them before they impact your daily activity. You’re in the right place if you want to learn how to prevent plantar fasciitis from developing.
But first, it’s important to learn the plantar fascia’s responsibilities. Understanding the injury helps you understand prevention and treatment techniques.
JACO Rehab has the best therapists to help you understand what’s happening. If you have questions, reach out!
What is Plantar Fascia?
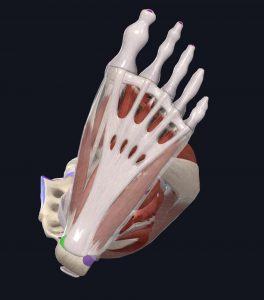
The plantar fascia is a sheet of soft tissue that spans the bottom of your foot. It attaches from your heel to the beginning of your toes and intertwines with many small muscles in the bottom of the foot. We call them “intrinsic” foot muscles. Because of the plantar fascia’s close relationship with the foot’s intrinsic muscular system, its structure resembles both tendon and ligament, which is unique to the body. (1)
Your plantar fascia is very thick and doesn’t stretch or shorten well, but that’s a good thing. A strong, thick plantar fascia are important for the health and function of the foot.
- The Plantar Fascia (white)
Images courtesy of Complete Anatomy
This thick structure also has a close relationship with the Achilles tendon, which attaches your calf muscles to the heel. A dysfunctional relationship between the two can cause pain, so keeping them healthy has an important role in overall foot health.
What Does the Plantar Fascia Do?
Your plantar fascia is responsible for creating an arch in your foot. The foot’s intrinsic muscles work with the fascia help raise the arch when you’re standing, walking, and running. This is particularly true when pushing off your big toe due to its muscles and their integration with the fascia.
Its thick nature helps distribute force during activity. It works together with the joints, muscles, and fat pads in your foot to absorb and propel force.
Like many structures in the body, the plantar fascia can take a beating… but not for long. Poor movement mechanics can place repetitive, unnecessary stress on the fascia. Over time, the fascia can fail and tear. Unfortunately, tears disrupt force absorption and cause pain.
Before you know it, you have a vicious cycle which can be hard to break. It’s hard to rest a foot because we use our feet all the time. That’s why plantar fascia can be stubborn to treat.
So, What Exactly is Planar Fasciitis?
Plantar fasci-“itis” was once believed to be an inflammatory response to stress on the body part. More recent research classifies this injury as a fasci-“osis” instead. The suffix “-osis” refers degeneration over time.
Degeneration is the scary medical term for wear and tear. That means the structure was probably handling undo stress long before it became symptomatic.
Plantar fasciitis (now fasciosis, but we will keep it fasciitis for now) is not something that happens overnight; you get it with time due to faulty body mechanics, which often involve stretching the fascia beyond its capacity repetitively. Some blame “flat feet,” but the cause depends on how the trunk, hips, knees, and ankles move together—not just one part of the body (more on this below). It’s gradual onset means treatment isn’t immediate, and surgery alone won’t always resolve the problem completely. Rehabilitating this injury takes time. We’re talking months, but it’s worth the effort to avoid going under.
The best rehab approach finds the root of the cause, then rebuilds movement habits in a way that will decrease stress on the fascia.
If you want to make sure you’re doing everything you can to prevent or treat your plantar fascia pain, make an appointment with our therapists at JACO Rehab before the injury impacts your daily routine.
What Does Plantar Fasciitis Feel Like?
Plantar fasciitis signs and symptoms are textbook. The painful areas and activities tend to be similar across the board, with some variation depending your unique circumstances.
Symptoms
- Pain at the bottom of the heel, particularly at the medial tubercle of the calcaneus, which is where doctors and physical therapists will look first.
- Pain first thing in the morning when standing out of bed, or pain when standing after sitting for a long period of time.
- Pain intensifies after walking, running, climbing stairs, which further stresses the structure.
Those who have (or are vulnerable to) plantar fasciitis will also have very tight calves. As mentioned earlier, the Achilles tendon attaches the heel to the calf musculature and is closely related to the plantar fascia. Tightness in the calves can increase stress on the fascia, contributing to pain.
- Typical Painful Spot (in green)
Images courtesy of Complete Anatomy
Myth: Only flat-footed people develop plantar fasciitis
Yes, it’s true that “flat feet” can cause increased stress on the fascia… but it doesn’t just happen to people with low arches!
Those with high arches can also develop plantar fasciitis.
The bones that are in the midfoot are meant to shift around. A flexible midfoot can help dissipate loads through the arch. High-arched feet tend to have a more rigid midfoot, which increases load through the fascia.
Let it be known that low and high arches can both develop plantar fasciitis due to faulty movement mechanisms! (1)
Exercises to Prevent Plantar Fasciitis
Okay, let’s get to the good stuff.
We now know that:
- The plantar fascia is meant to disperse load, but not by itself
- Plantar fasciitis is more accurately termed plantar fasciosis, which develops over time with repetitive stress from poor movement habits
- Tight calves and rigid arches are factors that can increase stress on the plantar fascia
Let’s use that information to prevent plantar fasciitis or treat mild plantar fascia pain before it gets worse.
The information below is just the start. If you have questions or need guidance, it’s best to see your physical therapist.
1. Strengthen the Intrinsics
There are very simple exercises you can do to strengthen the muscles that support your foot’s arch.
Remember, intrinsic muscles work very closely with the fascia. They can help offload the fascia when they are strong and active.
One exercise is the short-foot exercise. While keeping your foot flat on the ground, you’ll to lift your arch using only foot intrinsics. The ball of your foot should never leave the ground. Think of pushing your toes into the ground without scrunching, like you’re grounding your whole foot into the surface.
Try doing 25 good ones, holding for a few seconds each time. Practice twice per day in a standing position, if tolerated.
- Relaxed
- Arched
2. Stretch the Calves
Since tight calves are a predisposing factor to plantar fasciitis, let’s address it.
You have two muscles in your calf: the gastrocnemius and the soleus. They join at the Achilles tendon and attach at the heel.
Remember, the calf and the plantar fascia have a close relationship. Tight calves increase stress on the fascia.
Stretching the gastrocnemius looks slightly different than stretching the soleus. You stretch your gastrocnemius by keeping the knee straight, and you stretch your soleus by bending the knee slightly.
You should be stretching for at least 30 seconds twice per day.
- Stretch the gastrocnemius (knee straight)
- Stretch the soleus (knee bent)
3. Move the Midfoot
Even if your arches aren’t high, the midfoot can still get “stuck” if the bones aren’t moving well together.
Remember, a rigid midfoot doesn’t disperse force well, which displaces it on the plantar fascia.
You can move your midfoot around using your hands or a ball, depending on what’s more comfortable. If you’re in pain, a ball may feel too intense and could make symptoms worse.
The goal isn’t just to massage the foot here – it’s to shift the bones of the midfoot and get them moving.
You can take a few minutes to do this throughout the day.
- Wring foot with hands
Set the Priority
Plantar fasciitis is a problem that develops over time. Since it takes time to develop, it takes time to heal. Make sure you make foot health a priority so that the condition doesn’t go beyond your control.
But, if it does, you’re one phone call away from a great team of physical therapists who can help you out.
Why Won’t my Plantar Fasciitis Go Away?
Have you tried taking steps toward prevention and it just isn’t going away? Has it been slowly worsening from weeks to months?
The problem may not be at the feet. It could be higher up the movement chain. Often, there are contributing factors at the knee, hip, or trunk.
If you’re frustrated with persistent foot pain, you should get it checked by a physical therapist. They will look at the entire movement chain, not just the foot, to determine where the problems lie.
A physical therapist’s approach is historically helpful. Conservative/nonoperative approaches like physical therapy are 90% effective in resolution of pain after 3-6 months. (1)
Yes, months. You must be consistent and patient!
Frequently Asked Questions
What are the best shoes for plantar fasciitis?
A classic example of a question with a classic physical therapist answer: it depends!
When you’re in pain, barefoot walking can be uncomfortable and supportive shoes can help.
That’s not always true, though. Completely changing the soles of your shoes from a low to high arch (or vice versa) can cause other problems. That’s a big change that can shock your body.
There are also cases where over-the-counter insoles placed in your shoes can create more pressure on the heel, causing more pain.
The best shoe to wear is the most comfortable one you own. If there’s less pain wearing a specific slipper/sandal/shoe, wear it often. Then, take that shoe to the store and ask a retailer for shoes with a similar build.
Should I invest in orthotics?
You could invest in orthotics, but this is a costly treatment that may or may not work. Try the simple but long-winded treatments first, strengthening and stretching your body with therapist guidance for at least six weeks to give your body an opportunity to adapt. Orthotics don’t make you stronger; they support you and supplement muscle strength, similar to braces. It’s an accommodation that doesn’t treat the root cause in most cases.
For this reason, we also discourage orthotics as a prevention technique. Strengthen instead!
Does foot massage help plantar fasciitis?
It can, but you should be careful if your symptoms have flared. Massages to the painful areas could be too intense and cause increased pain.
It’s best to massage the foot yourself, if possible. Don’t start with massage guns, machines, or deep massage.
Avoid the heel if it’s painful. Instead, with light pressure, ease into the arch of your foot with your hands or a ball.
Deep friction massage may be employed by your physical therapist if they deem it appropriate for your specific presentation.
Prevent Plantar Fasciitis and Prioritize Foot Health!
Good luck preventing plantar fasciitis! If you need extra guidance, do not hesitate to contact the physical therapists at JACO Rehab.
Written by Nicole Hernandez, DPT
Sources
1. Latt LD, Jaffe DE, Tang Y, Taljanovic MS. Evaluation and Treatment of Chronic Plantar Fasciitis. Foot & Ankle Orthopaedics. 2020;5(1). doi:10.1177/2473011419896763